The AHI Best Practice Dentistry (AHI_BPD)
Dental Healthcare is provided at school setting adopting a modern biological approach to prevent and manage tooth decay.
The AHI has launched a new campaign to Eradicanting Dental Pain in Schoolchildren worldwide.
For this purpose AHI has developed a scalable, low-cost HPS model, piloted its implementation, and developed Guidelines to implementing and Protocols to assess the impact of the AHI-model of HPS. Available by request.
Words do not alleviate pain
It is rational to restore dental treatment as the foudation of Goverments action plans to address the current huge global burden of untreated dental caries in schoolchildren.
Clearly, a different stratech is urgently needed.
The prevalence of untreated dental caries remains static for more than 20 years, and the number of cases is increasing.
The AHI Best Practice Dentistry (BPD) integrates health promotion and clinical prevention. The primary intervention is detecting dental caries at early stages and intercepting decay progression through biological management of tooth decay at school setting.
Dentist time is to provide dental treatment.
Oral Health Promotion is provided by school teachers and incorporated into school daily life.
The AHI model integrates oral health promotion into school teaching and curative dental care at school settings. Dental care is delivered during breaks or study hours to minimize disruption in running the school curriculum.
Screening
All children undergo screening for untreated dental diseases, with clinical examinations recording indices widely used in epidemiology and treatment planning, including Sound, Decayed, Missing, Filled Teeth, PUFA, ICDAS II, and CAST categories [5].
Management of tooth decay
Fissure sealants are applied to newly erupted permanent molars and premolars [6]. Treatment follows the principles of minimally invasive dentistry, focusing on intercepting disease at early stages [7]. Techniques include sealing dentinal caries under adhesive restorations, sometimes after partial removal, and using the Atraumatic Restorative Treatment (ART) method, which employs hand instruments and glass ionomer cement without anesthesia or drilling [7–9].
AHI_BPD advocate using 38% silver diamine fluoride (SDF) to arrest caries in primary teeth [10]. SDF is non-invasive, inexpensive, and effective at halting disease progression, though it causes black staining of carious lesions and has an unpleasant metallic taste. Evidence indicates SDF is safe, effective, and suitable for school-based programs [10–12].
Management of Severe Disease
For advanced cases (e.g., unrestorable crowns, exposed pulps, or retained roots), AHI provides extractions to alleviate pain and prevent infection. Severe disease is rare in children aged 6–8 years, underscoring the importance of early intervention.
Life Skills and Health Literacy
School teaching aim to promote life skills and oral health literacy. Oral health literacy teaching highlight the benefits of healthy diets and oral hygiene. Life skills teaching focuses on psychosocial motivators to overcome the structural barriers to adopt a healthy lifestyle.
A series of four classroom sessions address each topic through a structured school-based teaching: Introduction of the topic via e-learning and a quiz game, a moderated debate one week later, group discussion in the following week and setting an individual goal for a behaviour change.
A Health Detective game is an epidemiological exercise to assesses learning in an entertaining way. School children, in partnership with their parents, take on the role of a detective and search for environmental and behavioural clues to the causes of disease in their home, school and/or community environment (‘investigating the crime’), collate and analyse the information collected (‘solving the crime’), identify potential solutions for the prevention of the occurrence of new cases of the disease (‘crime prevention’). The game promotes not only an understanding of the proximal causes of disease (e.g.: bacteria is the proximal cause of oral diseases) but also enables insight into the ‘causes of the causes’ of disease (e.g.: sugar consumption) and an awareness of the means for prevention (reduce sugar consumption, brush teeth with fluoridated toothpaste).
Promoting a Healthy Diet
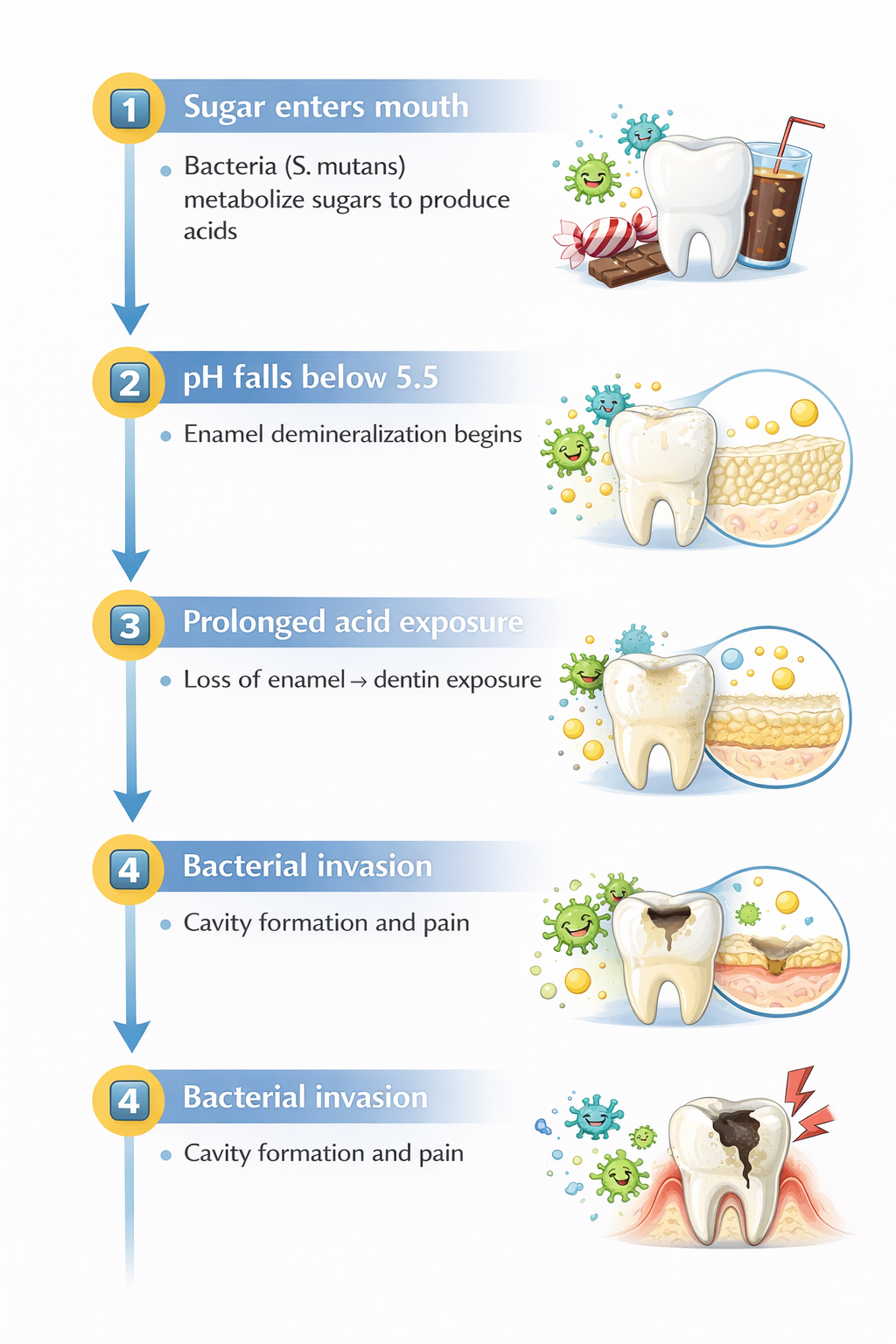
Sugar is the single most important dietary factor in the development of dental caries.
The current evidence strongly supports reducing both total sugar and frequency of intake, alongside fluoride-based prevention, as the most effective preventive strategy.
Promoting Oral Hygiene
AHI aligns with the WASH (Water, Sanitation, and Hygiene) framework [1] and adds supervised toothbrushing with fluoridated toothpaste in schools. This guarantees that children brush with fluoridated toothpaste at least twice daily. Evidence confirms that regular toothbrushing [2,3] and fluoride use [4] are the most effective preventive strategies against caries and periodontal diseases. Health promotion also includes providing healthy school meals and distributing nutritious food to families, addressing socio-economic barriers to healthy eating.
⸻
References
1. UNICEF. Strategy for water, sanitation, and hygiene 2016–2030. New York: UNICEF Programme Division; 2016.
2. Kumar S, Tadakamadla J, Johnson NW. Effect of toothbrushing frequency on incidence and increment of dental caries: a systematic review and meta-analysis. J Dent Res. 2016;95(11):1230–1236.
3. Lertpimonchai A, Rattanasiri S, Vallibhakara SA, Attia J, Thakkinstian A. The association between oral hygiene and periodontitis: a systematic review and meta-analysis. Int Dent J. 2017;67(6):332–343.
4. Marinho VC, Higgins JP, Sheiham A, Logan S. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst Rev. 2003;(1):CD002278.
5. Gudipaneni RK, Alkuwaykibi AS, Ganji KK, et al. Assessment of caries diagnostic thresholds of DMFT, ICDAS II and CAST in the estimation of caries prevalence in first permanent molars in early permanent dentition: a cross-sectional study. BMC Oral Health. 2022;22(1):133. doi:10.1186/s12903-022-02134-0
6. Mickenautsch S, Yengopal V. Caries-preventive effect of high-viscosity glass ionomer and resin-based fissure sealants on permanent teeth: a systematic review of clinical trials. PLoS One. 2016;11(1):e0146512.
7. Innes NP, Manton DJ. Minimum intervention children’s dentistry: the starting point for a lifetime of oral health. Br Dent J. 2017;223(3):205–213. doi:10.1038/sj.bdj.2017.671
8. Pitts N, Zero D. White paper on dental caries prevention and management: A summary of the current evidence and the key issues in controlling this preventable disease. FDI World Dental Federation; 2016.
9. Desai H, Stewart CA, Finer Y. Minimally invasive therapies for the management of dental caries: a literature review. Dent J (Basel). 2021;9(12):147. doi:10.3390/dj9120147
10. Gao SS, Zhao IS, Hiraishi N, et al. Clinical trials of silver diamine fluoride in arresting caries among children: a systematic review. JDR Clin Trans Res. 2016;1(3):201–210. doi:10.1177/2380084416661474
11. Contreras V, Toro MJ, Elías-Boneta AR, Encarnación-Burgos A. Effectiveness of silver diamine fluoride in caries prevention and arrest: a systematic literature review. Gen Dent. 2017;65(3):22–29.
12. Oliveira BH, Rajendra A, Veitz-Keenan A, Niederman R. The effect of silver diamine fluoride in preventing caries in the primary dentition: a systematic review and meta-analysis. Caries Res. 2019;53(1):24–32. doi:10.1159/000488686